| Covid-19 Blog |
Although the COVID-19 pandemic started in late 2019, it is still new to us because there’s a lot to learn about what the new coronavirus actually does to healthy lungs. The disease started when people developed pneumonia without any known cause. Later, Sars-CoV-2 that causes COVID-19 was found to be the cause of pneumonia.

COVID-19 causes the infection of the upper and lower respiratory tract, affecting the lungs. In severe cases, it causes lung complications, such as sepsis, ARDS (acute respiratory distress syndrome), pneumonia, and bronchitis. Infected people are the source of spreading the COVID-19 via the droplets when they sneeze, breathe, cough, or talk to someone.
The coronavirus symptoms appear when the virus enters the respiratory system through the nose and mouth. The damage caused by COVID-19 varies from person to person. Mild symptoms include tiredness, fever, and dry cough and appear in 80% of people. Respiratory failure, multi-organ system failure, and septic shock occur in 5% of people. 15% of people develop pneumonia, and only 2% of the cases can be life-threatening [1].
According to the World Health Organization (WHO), people with pre-existing health conditions like hypertension, cardiac problems, diabetes, and asthma, may experience severe symptoms of COVID-19. Some people infected with COVID-19 do not develop any symptoms (asymptomatic). Older people aged over 80 are more susceptible to die from COVID-19 [2].
Coronavirus And Your Lungs:

The virus affects your lungs by gaining entry into the body, where it destroys the mucous membrane of your mouth and nose. The virus starts replicating throughout the body and makes copies of itself [3].
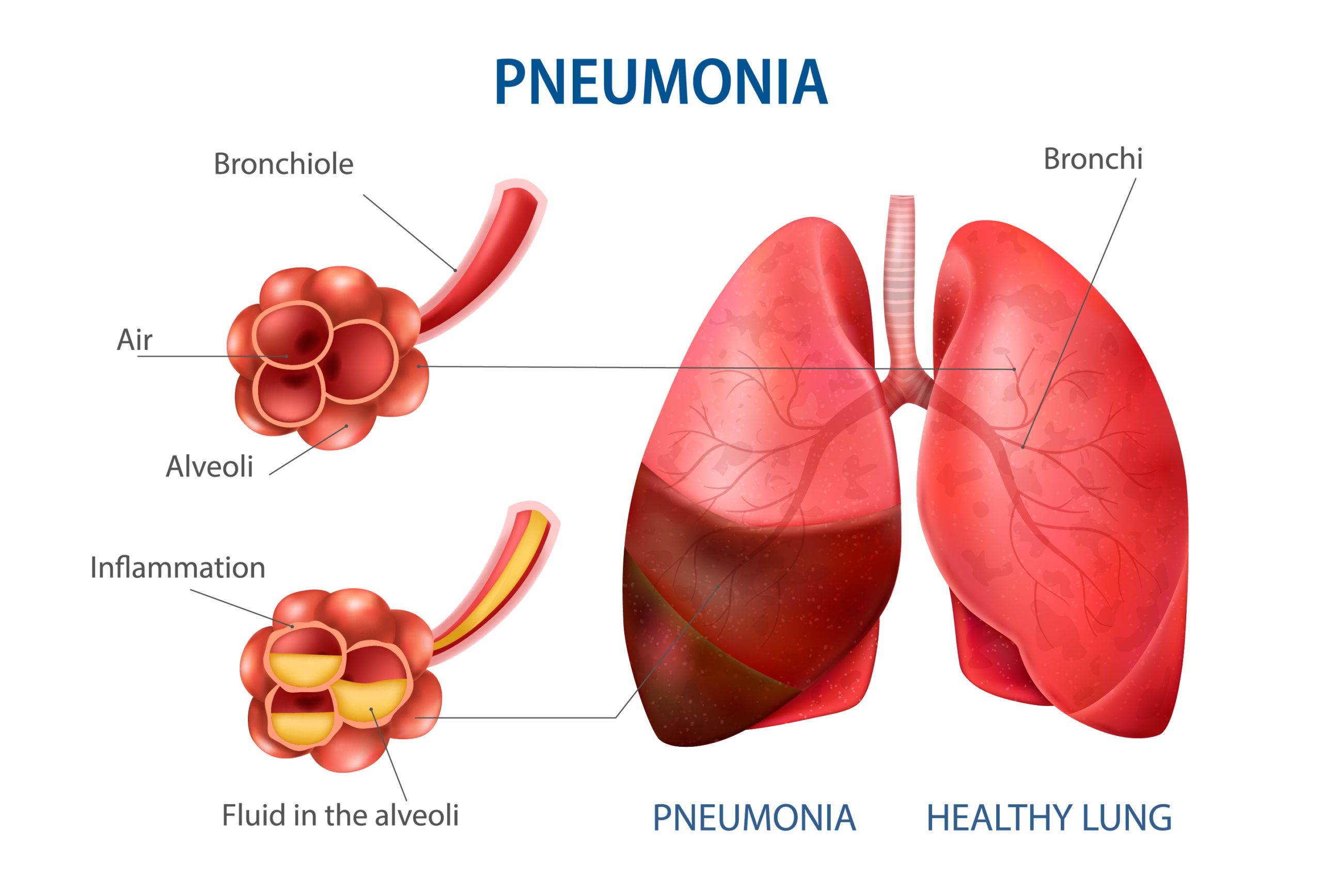
The structure of your respiratory tracts is just like an upside-down tree. The windpipe or trachea acts as a trunk of the tree, which acts as a passage for air. From the trachea, many smaller branches split in your lungs. In the lungs, each branch contains alveoli (tiny air sacs) at its end.
The lower airways of your respiratory tract contain ACE-2 receptors. This is where the coronavirus starts hijacking the healthy ACE-2 receptors and kills them. The lungs get infected and inflamed because the virus causes the fluid to fill up in the lungs, making it difficult for you to breathe [4].
Mild & Moderate Cases
As COVID-19 infects a person’s airways, it results in lung inflammation. As a result of inflammation and swelling, the immune response fights back. You may experience a dry cough, pain while breathing, sore throat, and chest tightness. Almost 80% of people exhibit mild to moderate symptoms of COVID-19.
Severe Cases
If inflammation increases in both lungs and swelling worsen, the lungs may fill with debris (from dead cells) and fluid. If this is the case, you might have pneumonia. Pneumonia causes the alveoli to be filled with fluid and mucus, thus affecting the impaired gas transfer and insufficient oxygen levels.
If very low levels of oxygen transfer into the bloodstream, the patient may be placed in the ICU. 15% of people exhibit severe cases of COVID-19.
Critical Cases
The most critical cases of COVID-19 are experienced by about 5% of people. In critical cases, your body tries to fight off the infection, but your lungs end up being more inflamed and swollen. Inflammation damages the alveoli and makes it difficult for air sacs to exchange oxygen and carbon dioxide.
The patients may need oxygen supply from a ventilator in critical cases, such as ARDS or pneumonia. In most critical cases, a patient may experience life-threatening consequences, e.g., clotting in the lungs, brain, and heart.
Types Of Damage In The Lungs Caused By Coronavirus
A patient may experience many lung complications caused by COVID-19, such as pneumonia, septic shock, bronchitis, and ARDS in severe cases. Read on to get to know about lung complications.
Pneumonia
When the coronavirus passes through the lining of airways, it infects gas exchange units – alveoli. Pouring of inflammatory material in the air sacs occurs due to inflammation; this is when a patient might end up having pneumonia.
The oxygen level with pneumonia becomes unable to enter into the bloodstream. The symptoms of pneumonia include tiredness, nose congestion, heavy sweating, dizziness, and rapid breathing [5].

Pneumonia caused by COVID-19 is more severe because it causes lasting lung damage, and it takes months for a patient to recover from it entirely.
Acute Respiratory Distress Syndrome (ARDS)
If pneumonia caused by COVID-19 becomes more severe, it causes the air sacs or alveoli to be more inflamed and filled with inflammatory material (which leaks from blood vessels in the lungs). The result is ARDS, which is characterized by increased heart rate, breathing difficulties, dry cough, and heavy breathing [6].
Patients with ARDS require oxygen supplementation through a ventilator or extracorporeal membrane oxygenation (ECMO). If ARDS continues to progress, it results in more critical complications, such as scarring of the lungs (fibrosis).
Bronchitis
If you have chronic bronchitis, you are more prevalent to the infection of COVID-19. When the epithelial lining of bronchial tubes (tubes through which the air passes to and from the lungs) is inflamed with bronchitis, the barrier that protects the lungs is destroyed.
The most common symptoms of bronchitis include dry cough, which gradually converts to mucus-containing cough. The less common symptoms might include chest discomfort, fever & chills, mild body aches, and fatigue.
Septic Shock
In septic shock, the body’s reaction to inflammation goes off the target, as a result of which, the infection keeps spreading into the bloodstream, damaging every tissue. As there’s a close relationship between the heart and the lungs, septic shock negatively affects these organs [7]. Even if the septic shock is treated, the patients end up having lasting lung damage.
Improve Your Lung Health After Covid-19:
Recovering from the COVID-19 can be distressing because improving a decline in lung function is also a battle. There are several ways through which you can recover your lung health after COVID-19.
- Breathing Exercises: An obstructed flow of oxygen and breathlessness are the two main symptoms, which decline lung capacity. Meditative postures and deep breathing exercises greatly help you improve your lung function. Pursed-lip breathing exercise also helps strengthen your lungs after bronchitis.
- Avoiding Pollution: If your lung function has been compromised by COVID-19, you should avoid exposure to a polluted environment. You may get reinfection due to the pollution and smoke.
- Quit Smoking: Your lungs become more vulnerable to infection when you smoke. Smoking increases your risk of infection and transmission of COVID-19. Excessive smoking and tobacco reduce your lung capacity and cause pulmonary infections.
References:
- Jung F, Krüger-Genge A, Franke RP, Hufert F, Küpper JH. COVID-19 and the endothelium. Clin Hemorheol Microcirc. 2020;75(1):107–19.
- Kim G -u., Kim M-J, Ra SH, Lee J, Bae S, Jung J, et al. Clinical characteristics of asymptomatic and symptomatic patients with mild COVID-19. Clin Microbiol Infect [Internet]. 2020;26(7):948.e1-948.e3. Available from: https://www.sciencedirect.com/science/article/pii/S1198743X20302688
- Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: A review. Clin Immunol [Internet]. 2020;215:108427. Available from: https://www.sciencedirect.com/science/article/pii/S152166162030262X
- Dalan R, Bornstein SR, El-Armouche A, Rodionov RN, Markov A, Wielockx B, et al. The ACE-2 in COVID-19: Foe or Friend? Horm Metab Res [Internet]. 2020/04/27. 2020 May;52(5):257–63. Available from: https://pubmed.ncbi.nlm.nih.gov/32340044
- Lee EYP, Ng MY, Khong PL. COVID-19 pneumonia: what has CT taught us? Lancet Infect Dis [Internet]. 2020;20(4):384–5. Available from: http://dx.doi.org/10.1016/S1473-3099(20)30134-1
- Gattinoni L, Chiumello D, Rossi S. COVID-19 pneumonia: ARDS or not? Crit Care [Internet]. 2020;24(1):154. Available from: https://doi.org/10.1186/s13054-020-02880-z
- Prescott HC, Girard TD. Recovery From Severe COVID-19: Leveraging the Lessons of Survival From Sepsis. JAMA [Internet]. 2020 Aug 25;324(8):739–40. Available from: https://doi.org/10.1001/jama.2020.14103