The Myths Associated with Cholesterol and their Facts
| The Cholesterol Paradox Blog |

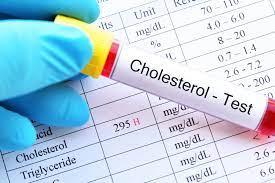
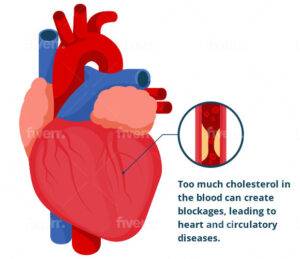
American children and adults with high cholesterol average about 7% and 21%, respectively. Having no symptoms, high cholesterol can be challenging to detect without blood work, yet the hazards are real. It has been discussed in the previous blogs that having high cholesterol along with other risk factors can raise your chance of developing heart disease. It is also necessary for your body to make vitamin D, digest food, absorb vital minerals, and more (1).
Even though most people are aware of cholesterol, there are still a lot of misconceptions about it. Don’t worry because we are here to correct your misconceptions. This post has reviewed the most recent findings and information regarding cholesterol. This blog will clear your queries regarding cholesterol.
Myth
High Cholesterol Food is always responsible for Cardiovascular Complications
Fact
Diet culture frequently blames food, glorifying some foods while demonizing others. Numerous foods high in fatty acids and related to heart disease include red meats, dairy products, and other foods that are also high in cholesterol. According to recent studies, foods with high cholesterol but low-fat content, such as eggs and shrimp, do not cause heart disease. The discussion of cholesterol is further complicated by the identical structural characteristics of ingested cholesterol and cholesterol produced by the liver.
The cholesterol in meals is comparable to the cholesterol our bodies manufacture. Plants cannot synthesize it; hence it can only be found in animal products. Even though we can absorb cholesterol through the digestive system, only around 10% of dietary cholesterol affects our blood. Any food that contains calories, such as foods high in protein, carbs, fats, or alcohol, causes the liver to make the cholesterol found in our blood. Triglycerides, the primary fat found in our food and bodies, is also bundled with protein to form cholesterol.
Your body is remarkably adept at self-regulating: When you consume less dietary cholesterol, your body produces more to make the difference. Your body produces less cholesterol naturally when you consume more of it. Additionally, dietary cholesterol doesn’t appear to raise people’s risk of heart disease, even though it may slightly raise LDL in some individuals (2).
Myth
The sole source of cholesterol is our diet
Fact
While animal commodities, such as meat, fish, eggs, and whole milk, can contain cholesterol, your liver also naturally manufactures cholesterol. Some individuals produce more cholesterol in their livers than they require due to certain reasons such as genetics or any other disease. High cholesterol is possible in certain circumstances, but a balanced diet and careful management prevent it (3).

You may wonder if cholesterol is obtained only from animal sources, then vegans do not have any chance of having high cholesterol. You can be wrong here. The fact is that a vegan has the same chance of developing high cholesterol as a person who eats meat. This is because the real cause of health issues is inflammation caused by high carbohydrate consumption.
Myth
Only egg whites have benefits, and yolks are not our good folks
Fact
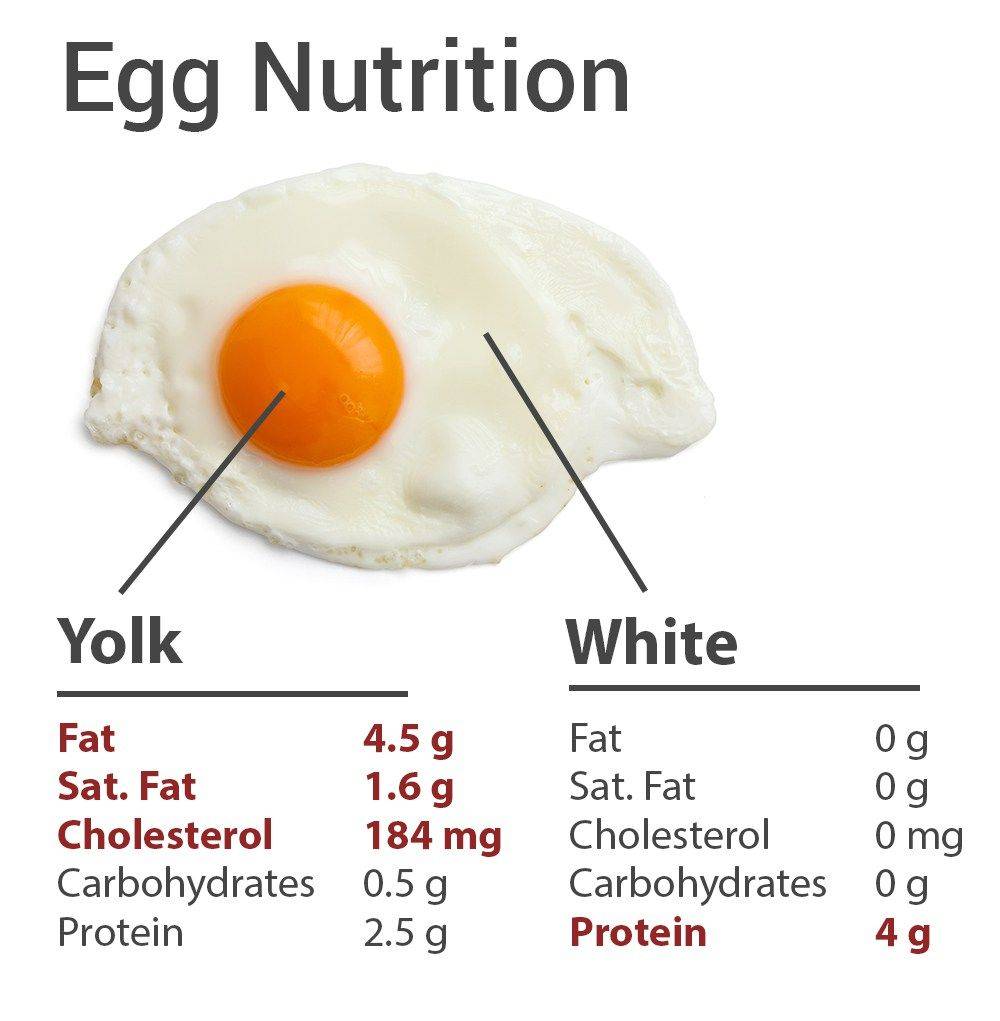
According to Stewart, “Natural and farm eggs are a high protein supply and rich in a variety of vitamins and minerals.” Egg white provides some protein (about two grams). Most of an egg’s iron, biotin, folate, and vitamins A, D, E, and K are found in the egg yolk, along with around four grams of protein.
One ground-breaking 2013 study examined the effects of consuming whole eggs vs. an equivalent amount of a yolk-free egg substitute on blood cholesterol. Three months later, those who consumed three whole eggs daily had higher HDL levels and lower LDL levels than those who used egg substitutes.
You don’t have to avoid eggs as long as you consume them in moderation (4). The American Heart Association advises a daily intake of no more than 300 mg of dietary cholesterol. Up to 200 mg, or more than two-thirds of the advised amount, can be found in eggs. As a quick reminder, your body is working for you. The cholesterol level in your bloodstream is constrained if your nutritional intake increases since your body create less cholesterol.
Myth
All types of cholesterol are harmful to our body
Fact
Although excessive cholesterol is frequently discussed, not all cholesterol is harmful, as discussed in detail in the previously published article. In fact, according to the CDC, your body needs it for several essential processes like creating hormones and cells. Even our liver produces some.
The majority of research currently demonstrates that for the majority of people, dietary cholesterol does not significantly affect blood cholesterol, contrary to what medical professionals traditionally believed. Our body produces and controls the amount of cholesterol needed to perform critical tasks like making hormones and serving as a crucial component of cell membranes,
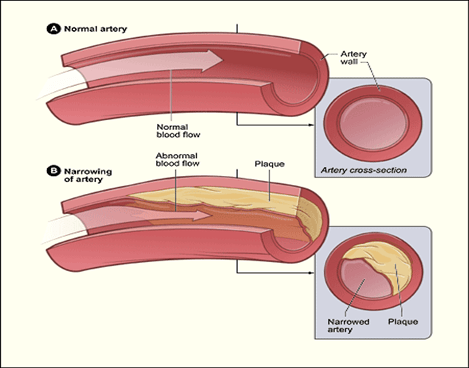
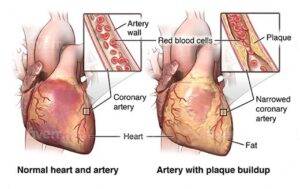
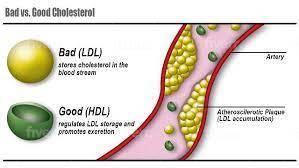
Different varieties of cholesterol exist. Unfortunately, the majority of the cholesterol in your body is the “bad” type of cholesterol, low-density lipoprotein (LDL), as already discussed in previous articles of this series. LDL can adhere to the blood vessel walls. Heart disease and stroke risk may increase due to this plaque buildup.
Your blood also contains high-density lipoprotein (HDL), a “healthy” type of cholesterol. Cholesterol is taken up by HDL and sent to the liver for processing. Thus, your risk of heart disease and stroke is decreased by HDL (5).
Myth
It would be best if you avoided cholesterol in your diet as much as you can
Fact
“The current nutrition guidelines no longer list dietary cholesterol as one of the “nutrients to limit.” The majority of the top-quality animal products are exceptionally nutrient-dense. You miss out on many health-promoting elements if you eliminate all or most dietary cholesterol. Blood cholesterol levels are not significantly affected by dietary cholesterol. Instead, it is more affected by the quantity and kind of fats you ingest. Consuming excessive amounts of trans and saturated fats will increase your cholesterol.
Eggs and shellfish, which are foods rich in dietary cholesterol, are excellent sources of lean protein and probably have less influence on cholesterol levels than many manufactured snack foods. For instance, grass-fed yogurt offers calcium and bacteria that help the gut repair, as well as iron and B vitamins that are abundant in grass-fed cattle.
Foods containing some cholesterol shouldn’t be quickly condemned because only 10% of that dietary cholesterol affects our cholesterol. Saturated fats, primarily in animal products with high-fat content, should be avoided as much as possible.
A complete 100% saturated fat compared to 10% dietary cholesterol can affect the liver’s ability to produce cholesterol. The American Heart Association (AHA) advises aiming for six percent or less of your daily caloric intake to come from sources of saturated fat, which include:
- butter
- cheese
- lard
- pork
- heavy cream
- skin-on poultry
- lamb
- beef
Myth
The products with a claim of being cholesterol free are healthy for us
Fact

This claim can be found in various products, including chocolate sandwich cookies and potato chips with cream filling. Food businesses frequently employ popular nutrition phrases to capture your interest and promote the consumption of the goods, with ‘cholesterol-free’ being one prominent example. Any meal that doesn’t include meat or dairy products with a lot of fat could be labeled as “cholesterol-free.”
Do highly processed, nutrient-deficient foods suddenly qualify as healthy?
Nope!
Aim to use various colors and plants in your dishes, along with some lean protein, healthy fats, and whole grains, rather than focusing on specific product promises. Another prevalent concept that must be addressed is that food that does not contain cholesterol is good for your heart. Even foods low in cholesterol or lacking in cholesterol may contain large amounts of saturated or trans fats, increasing your cholesterol levels.
Myth
Exercise and diet are enough to lower my cholesterol level in whichever state I am
Fact
Exercise and diet should be adopted in the first place and must be included in your daily routine. Despite the importance of diet and exercise, many people still require medicine. You may require cholesterol medications known as statins if you have type 2 diabetes, heart disease, a family history of high cholesterol, or any of these conditions (6).
Myth
Only overweight people have high cholesterol
Fact
Any person, irrespective of his weight, can have high cholesterol. High cholesterol can affect anyone, whether lean or overweight, while overweight people are more prone to have it. Adults of all ages require routine cholesterol testing. According to the American Heart Association, everyone over 20 should get their cholesterol levels examined every four to six years.
Myth
High cholesterol is not bad for kids but only for adults
Fact
Children with familial hypercholesterolemia, an inherited form of elevated cholesterol, are at an increased risk of developing heart disease. Ask your pediatrician whether you ought to have your child’s cholesterol checked. Additionally, all children can profit from a head start on a healthy diet and way of life, lowering the chance of developing heart issues.
Myth
The cereals such as OATS, high in fiber, are an excellent source to reduce cholesterol levels
Fact
According to research, oatmeal contains many fibers and can only help decrease cholesterol. The appropriate kinds of fats and fiber may have a more significant impact. The first dietary modification advised to lower cholesterol is reducing your intake of incredibly saturated fats.
Myth
The only way to lower cholesterol is by taking medicine
Fact

Maintaining healthy cholesterol levels requires leading a healthy lifestyle. Increased physical activity, a nutritious diet rich in fresh fruits and vegetables, and giving up smoking can all help lower cholesterol levels in people who already have high cholesterol or are at risk of getting it. However, some people’s high cholesterol will persist despite any lifestyle modifications they make. A doctor may recommend cholesterol-lowering drugs in these circumstances.
Myth
Women have low chances of heart disease than men
Fact
Both sexes have comparable rates of high cholesterol. Therefore, heart disease should be a worry for everyone. The Statistics show that heart disease is the leading cause of mortality for American women, killing one in five. Knowing the symptoms is important because women’s heart disease might manifest differently (7).
References
1. Ravnskov, U. Cholesterol Myths. (New Trends Publishing, Incorporated, 2003).
2. Vomero, J., Center, H. & Vomero, C. D. J. Cholesterol Myths–Is Cholesterol Really That Bad?
3. Ma, H. & Shieh, K.-J. Cholesterol and human health. J. Am. Sci. 2, 46–50 (2006).
4. Dawber, T. R., Nickerson, R. J., Brand, F. N. & Pool, J. Eggs, serum cholesterol, and coronary heart disease. Am. J. Clin. Nutr. 36, 617–625 (1982).
5. Wald, N. J. & Law, M. R. Serum cholesterol and ischaemic heart disease. Atherosclerosis 118, S1–S5 (1995).
6. Mattson, F. H., Erickson, B. A. & Kligman, A. M. Effect of dietary cholesterol on serum cholesterol in man. Am. J. Clin. Nutr. 25, 589–594 (1972).
7. Kromhout, D. Body weight, diet, and serum cholesterol in 871 middle-aged men during 10 years of follow-up (the Zutphen Study). Am. J. Clin. Nutr. 38, 591–598 (1983).



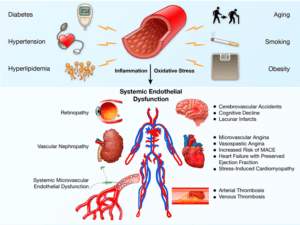
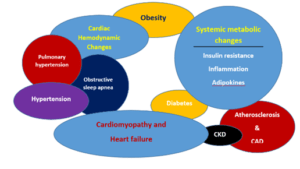
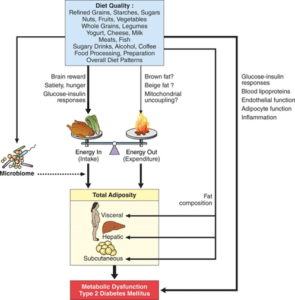
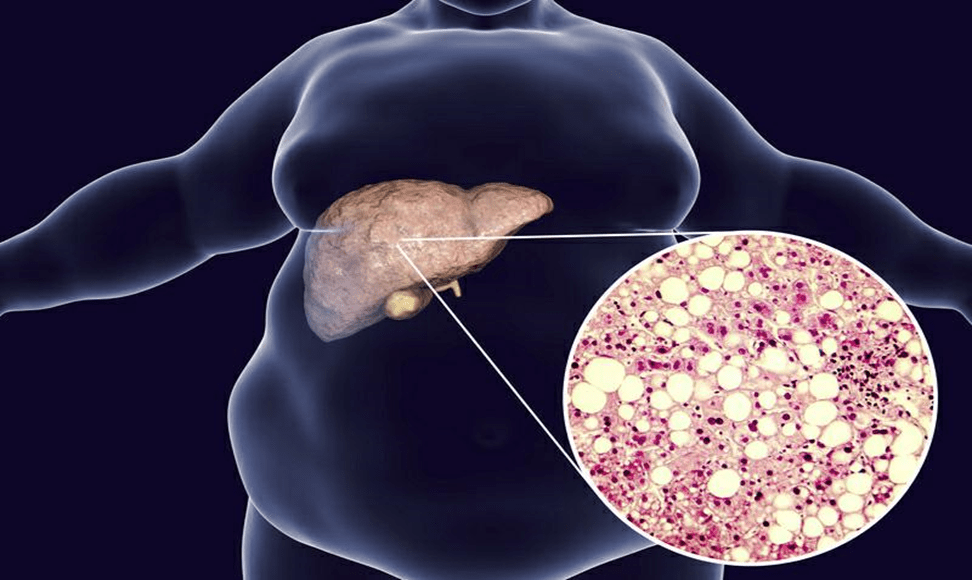
 Metabolic syndrome consists of a group of diseases. It includes the presence of a cluster of risk factors such as abdominal obesity, high blood pressure, impaired fasting blood glucose, high triglycerides, and low HDL cholesterol. The NHLBI (National Heart, Lung and Blood Institute) and AHA (American Heart Association) recommend that when one has 3 or more of these factors, he or she is said to have metabolic syndrome. Increased non-HDL cholesterol levels contribute to metabolic syndrome development (4). Metabolic syndrome affects health badly and increases the susceptibility to high blood pressure, diabetes, heart disease, and stroke (5).
Metabolic syndrome consists of a group of diseases. It includes the presence of a cluster of risk factors such as abdominal obesity, high blood pressure, impaired fasting blood glucose, high triglycerides, and low HDL cholesterol. The NHLBI (National Heart, Lung and Blood Institute) and AHA (American Heart Association) recommend that when one has 3 or more of these factors, he or she is said to have metabolic syndrome. Increased non-HDL cholesterol levels contribute to metabolic syndrome development (4). Metabolic syndrome affects health badly and increases the susceptibility to high blood pressure, diabetes, heart disease, and stroke (5).


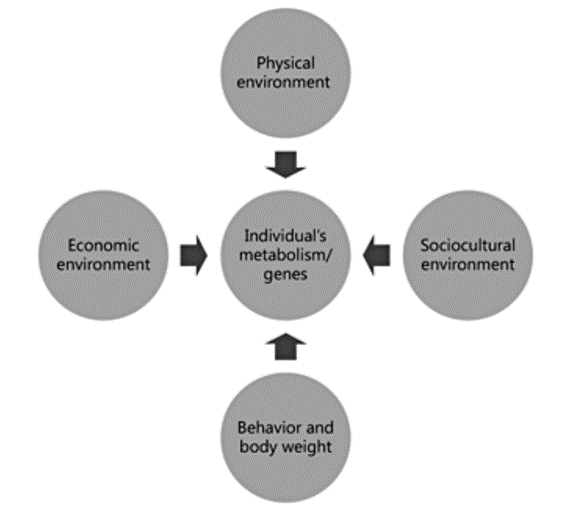
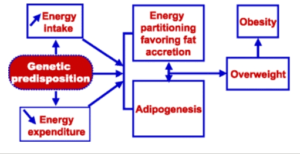

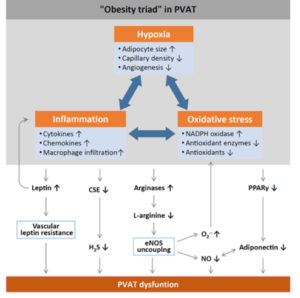
 Obesity is becoming a global epidemic, and there has been a dramatic increase in obesity cases among children and adults in the past 10 years. Obesity is an independent risk factor for cardiovascular disease and is associated with an increased risk of mortality and morbidity. As adipose tissue accumulates in excess amounts, various adaptations occur in cardiac structure and function. On the whole, obesity is associated with various cardiac complications such as coronary heart disease, heart failure, and sudden death because of its impact on the cardiovascular system. (1)
Obesity is becoming a global epidemic, and there has been a dramatic increase in obesity cases among children and adults in the past 10 years. Obesity is an independent risk factor for cardiovascular disease and is associated with an increased risk of mortality and morbidity. As adipose tissue accumulates in excess amounts, various adaptations occur in cardiac structure and function. On the whole, obesity is associated with various cardiac complications such as coronary heart disease, heart failure, and sudden death because of its impact on the cardiovascular system. (1)