Dietary And Exercise Tips To Lose Body Fats | A Comprehensive Guide
|
Body Fat Percentage Blog II |
In this Day and Age, almost everyone is concerned about their appearance, presentation, health, and diet. This increasing perceptive and insightful approach of people has led them to know more about their bodies, their anatomy, composition, and physiology so that they can look for ways to make them healthier, efficient, and beautiful. In this regard, Body fat plays a significant role as it happens to increase, and serious problems arise with its increase.
Body fat percentage is defined as the total mass of fat divided by total body mass multiplied by 100. (1)
The most common causes of obesity are overeating and physical inactivity. However, body weight and its composition result from genetics, metabolism, environment, behaviour, and culture. (2)
Diet tips for reducing body fat:
Our body responds to everything that we eat. The nutrients in our food determine the health of every cell of every tissue of every organ of the whole body. For this reason, we should remain careful and vigilant about what we eat or drink.
Low Energy Diets:
In order to lower the body fat percentage, we have to cut down the fat intake and switch to low-calorie or low-energy diets. Low-energy diets (LED) and very-low-energy diets (VLED) are categorized by the provision of 800– 1200 kcal/day and 400–800 kcal/day, respectively. Very low-energy diets are typically in liquid form and commercially prepared. The diet aims to induce rapid weight loss (1.0– 2.5 kg/week) (3)
Low-fat Diet:
You can simply start a low-fat diet to lower the body fat percentage. Low-fat diets (LFD) provide 20– 35% fat. This Low-fat diet is based on the Acceptable Macronutrient Distribution Ranges (AMDR) for adults.
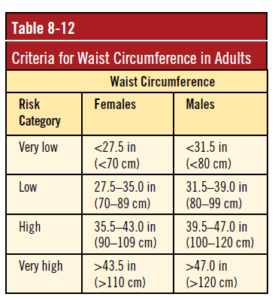
Lowering the proportion of dietary fat compared to usual intake modestly but consistently reduced body weight, body fat, and waist circumference. (3)
This diet plan has been proven to be very efficient in weight reduction.
Low carbohydrate diet:
Like Low-Fat diets, low-carbohydrate diets (LCD) are also a broad class lacking an objective definition. There is no universal arrangement of what quantitatively symbolizes an LCD. The AMDR lists 45–65% of total energy as the proper carbohydrate intake for adults. Therefore, diets with intakes below 45% lack the ‘official’ guidelines and can be viewed as LCD (3)
Ketogenic Diet:
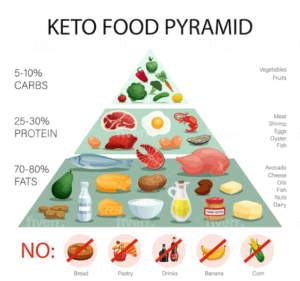
A ketogenic diet is objectively defined by its ability to raise circulating ketone bodies measurably.
A state called ketosis, also known as nutritional ketosis. Unlike completely fasting, this condition is attained by restricting carbohydrates to about ~50 g or ~10% of total energy while keeping protein restrained (1.2–1.5 g/kg/d), with the prevalence of energy intake from fat. (3)
Figure 4: Ketogenic Diet Chart (12)
High Protein Diet:
For a healthy diet, a high protein diet is paramount.
A common feature of high-protein diets (HPD) is that they have various subjective definitions. High-protein diets are generally defined as intakes reaching or exceeding 25% of total energy. Protein is the most satiating nutrient, followed by carbohydrates, and fat is the least. (3)
Intermittent Fasting:
One alternative method of caloric restriction is intermittent fasting, a broad term that encompasses several specific fasting protocols. The common theme among intermittent fasting protocols is that individuals periodically abstain from eating for periods longer than the typical overnight fast. These programs typically lead to energy restriction, but the restriction is not necessarily maintained daily. (4).
The majority of popular intermittent fasting protocols can be grouped into 1 of 3 categories: alternate day fasting, whole-day fasting, and time-restricted feeding. Each form of intermittent fasting utilizes different periods of feeding and fasting. (4)
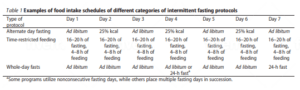
Figure 4: Food Intake Schedule of Intermittent Fasting (13)
Exercise tips for reducing body fat:

If a person’s body is healthy, active and strong, so is his mind. It is important to note that the relationship between physical activity and health, particularly in disease prevention, is not a new concept. (9)
Focusing on body composition is essential because even more important than overall weight loss is sustainably losing fat mass (FM) while maintaining lean body mass (LBM). (3)
Exercise – A way of energy expenditure:
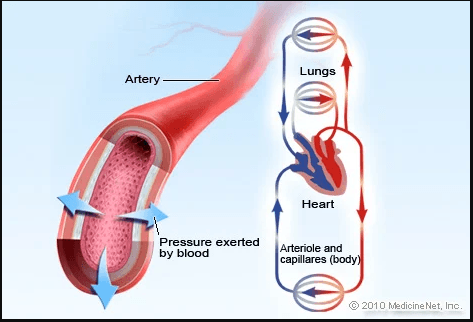
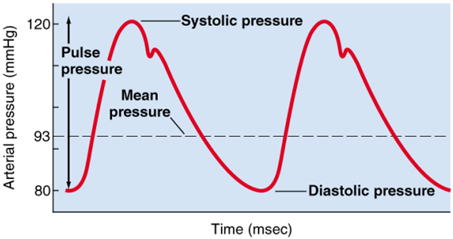
Exercise is commonly used as a weight loss method by increasing energy expenditure (EE) to create a sustained energy deficit. However, the issue of compensatory responses is more interesting, which undermines the exercise’s ability to promote theoretical weight loss. (7) Exercise benefits weight loss and helps maintain efficient body functions. Exercise delivers oxygen and nutrients to your tissues and helps your cardiovascular system work more efficiently.
Figure 5: Benefits of Lower Body Workout (14)
Different Useful exercises:
Many exercises help maintaining normal body functions, efficient blood circulation, great metabolism, good gastric and intestinal function, and excellent bone and muscle strength.
Aerobic exercises, e.g., jogging, skipping, etc., and resistance exercise use of free weights, weight machines, etc., have been shown to reduce adolescent body fat. (5) it can be expected that in a middle-aged person, a single exercise duration of more than 40 min would be more helpful in causing physiologically desirable changes. (6)
Circadian relationship with exercise:
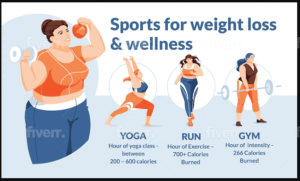
The time during which the exercise is performed is also important as it directly affects weight loss, as shown by studies.
Individuals who perform more exercise sessions in the morning have significantly greater weight reductions than those who perform more exercise sessions in the evening. (8)
Figure 6: Sports for weight loss and wellness (15)
Lifestyle tips for reducing body fat:
Eating healthy diets and exercising regularly is fruitless as long as you cannot let go of your sedentary and unhealthy lifestyle. A healthy diet, Healthy exercise and a Healthy lifestyle make you live longer, healthier and better.
More recent interest in the importance of physical activity to health has been predicated on the significant and progressive lifestyle changes experienced in the developed world over recent centuries and the developing world in recent decades. (9)
Relationship of a sedentary lifestyle with Non-communicable diseases:
The recently documented increase in physical inactivity, sedentary behaviours, and associated impact has been a concomitant increase in non-communicable diseases. Non Communicable Diseases account for an estimated 60% of all deaths and 44% of premature deaths and are thought to be the greatest cause of morbidity and mortality, even in the developing world. (9)
A sedentary lifestyle is a major adaptable risk factor for cardiovascular disease and other chronic diseases, including cancers, obesity, hypertension, bone and joint diseases, osteoporosis and osteoarthritis, type 2 diabetes and depression. (9)
Factors contributing to Sedentary Lifestyle:

Major environmental and lifestyle factors contributing to the physical activity and nutrition transitions include increased urbanization, industrialization, increased availability of labour-saving devices and new technologies along with the availability of poor quality, high-fat, and energy-dense foods. . Poor body composition, as reflected in excess body fat, is widely acknowledged as one of leading present-day global health threats and as a major risk factor for the more prominent chronic conditions—type 2 diabetes, cardiovascular disease, and hypertension. (9)
Figure 7: Effective Tips for Weight Loss (16)
How to Improve?
The lifestyle practices of many societies are characterized by low levels of habitual physical activity in combination with a poor diet. To improve your condition, follow the following steps:
|
1. Measure and Watch Your Weight. |
|
2. Limit Unhealthy Foods and Eat Healthy Meals. |
|
3. Take Multivitamin Supplements. |
|
4. Drink Water and Stay Hydrated |
|
5. Be Physically Active |
|
6. Reduce Sitting and Screen Time |
|
7. Get Enough Good Sleep |
|
|
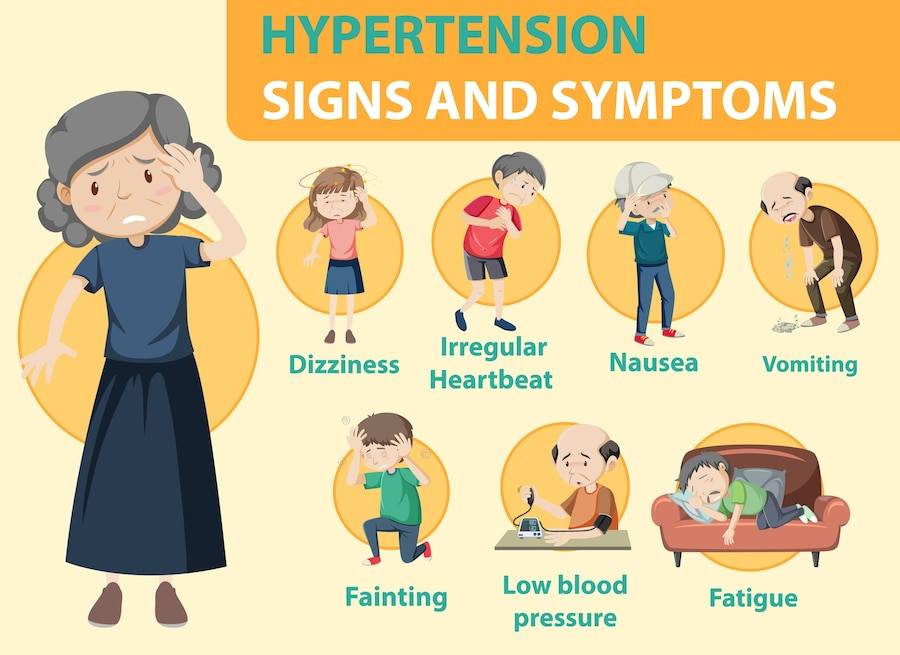
When to see a doctor:
By taking all of the above measures, if your body does not show any response, it is feasible for you to go to your doctor or physician. People suffering from some underlying disease may show symptoms different from others, making them liable for some medical interference. It is suggested that you go to your doctor immediately and get yourself checked If your body shows the following symptoms:
|
1. Sweating |
|
2. Tiredness |
|
3. joint and back pain |
|
4. difficulty breathing |
|
5. sleep problems, including snoring |
|
6. difficulty with physical activity |
|
7. low confidence and feelings of isolation |
|
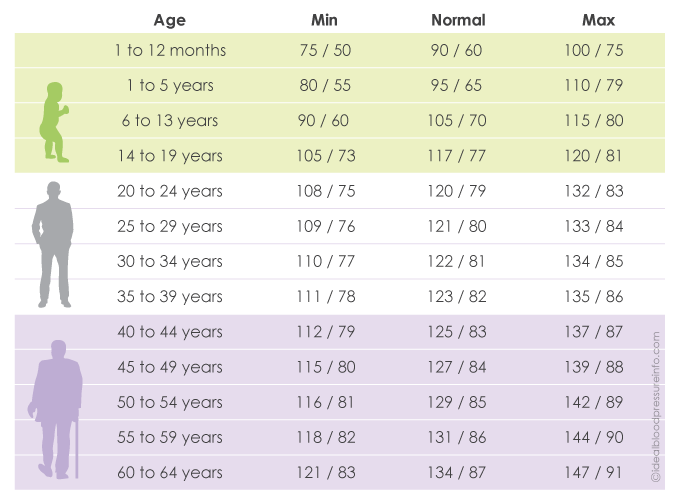
8. high blood pressure |
FAQs:
- What is body fat percentage?
- What are the methods of measuring the body fat percentage?
- What are the methods for lowering the body fat percentage?
- What can diet be adopted to lower body fat?
- What exercises should be done to lower body fat?
- What lifestyle changes should be made to lower body fat?
- When should we see a doctor?
Conclusion:
Studies show losing as little as 5% of your body weight can improve your health in many ways.
Lowering the body fat percentage reduces adipose tissue, which allows the body to manage blood sugar more effectively. Obese individuals are more likely to suffer from sleep apnea, a disorder characterized by interrupted breathing while sleeping. Excess body weight can increase fat deposits in your neck, obstructing the airways. Some studies show that weight loss can improve mood and self-confidence. Excess weight can cause wear and tear to joints which become stressed, damaged, and inflamed but losing weight can help. Losing weight can also improve your heart
Excess body weight is thought to cause about 11% of cancers in women and about 5% in men.
All these problems can be solved by reducing your body fat percentage. But, before you start any weight loss regime, it’s important to talk with your doctor about the right plan and goals for you.
References:
(1) Choe, Sung Sik; Huh, Jin Young; Hwang, In Jae; Kim, Jong In; Kim, Jae Bum (2016). Adipose Tissue Remodeling: Its Role in Energy Metabolism and Metabolic Disorders. Frontiers in Endocrinology, 7(), –. doi:10.3389/fendo.2016.00030
(2)Willoughby, Darryn; Hewlings, Susan; Kalman, Douglas (2018). Body Composition Changes in Weight Loss: Strategies and Supplementation for Maintaining Lean Body Mass, a Brief Review. Nutrients, 10(12), 1876–. doi:10.3390/nu10121876
(3) Aragon, Alan A.; Schoenfeld, Brad J.; Wildman, Robert; Kleiner, Susan; VanDusseldorp, Trisha; Taylor, Lem; Earnest, Conrad P.; Arciero, Paul J.; Wilborn, Colin; Kalman, Douglas S.; Stout, Jeffrey R.; Willoughby, Darryn S.; Campbell, Bill; Arent, Shawn M.; Bannock, Laurent; Smith-Ryan, Abbie E.; Antonio, Jose (2017). International society of sports nutrition position stand: diets and body composition. Journal of the International Society of Sports Nutrition, 14(1), 16–. doi:10.1186/s12970-017-0174-y
(4) Tinsley, Grant M.; La Bounty, Paul M. (2015). Effects of intermittent fasting on body composition and clinical health markers in humans. Nutrition Reviews, (), nuv041–. doi:10.1093/nutrit/nuv041
(5) Alberga, A S; Prud’homme, D; Kenny, G P; Goldfield, G S; Hadjiyannakis, S; Gougeon, R; Phillips, P; Malcolm, J; Wells, G; Doucette, S; Ma, J; Sigal, R J (2015). Effects of aerobic and resistance training on abdominal fat, apolipoproteins and high-sensitivity C-reactive protein in adolescents with obesity:the HEARTY randomized clinical trial. International Journal of Obesity, (), –. doi:10.1038/ijo.2015.133
(6) Seong-Hi Park;Chul-Gyu Kim; (2021). Effects of aerobic exercise on waist circumference, VO<sub>2</sub> max, blood glucose, insulin and lipid index in middle-aged women: A meta-analysis of randomized controlled trials . Health Care for Women International, (), –. doi:10.1080/07399332.2021.1900190
King, N. A.; Horner, K.; Hills, A. P.; Byrne, N. M.; Wood, R. E.; Bryant, E.; Caudwell, P.; Finlayson, G.; Gibbons, C.; Hopkins, M.; Martins, C.; Blundell, J. E. (2012). Exercise, appetite and weight management: understanding the compensatory responses in eating behaviour and how they contribute to variability in exercise-induced weight loss. British Journal of Sports Medicine, 46(5), 315–322. doi:10.1136/bjsm.2010.082495
(8) Willis, Erik A.; Creasy, Seth A.; Honas, Jeffery J.; Melanson, Edward L.; Donnelly, Joseph E. (2019). The effects of exercise session timing on weight loss and components of energy balance: midwest exercise trial 2. International Journal of Obesity, (), –. doi:10.1038/s41366-019-0409-x
(9) Hills, Andrew P. (2015). [Advances in Food and Nutrition Research] || Physical Activity and Health: “What Is Old Is New Again”. , (), –. doi:10.1016/BS.AFNR.2015.06.001
(10) Figure 1 retrieved from Willoughby, Darryn; Hewlings, Susan; Kalman, Douglas (2018). Body Composition Changes in Weight Loss: Strategies and Supplementation for Maintaining Lean Body Mass, a Brief Review. Nutrients, 10(12), 1876–. doi:10.3390/nu10121876
(11) Figure 2 retrieved from https://www.pinterest.com/pin/332562753746418488/
(12) Figure 3 retrieved from https://www.freepik.com/premium-vector/realistic-keto-diet-pyramid-infographics-with-percentage-fats-protein-carbs-prohibited-food-illustration_16608066.htm
(13) Figure 4 retrieved from Willoughby, D., Hewlings, S., & Kalman, D. (2018). Body Composition Changes in Weight Loss: Strategies and Supplementation for Maintaining Lean Body Mass, a Brief Review. Nutrients, 10(12), 1876. https://doi.org/10.3390/nu10121876
(14) Figure 5 retrieved from https://www.stylecraze.com/
(15) Figure 6 retrieved from https://www.freepik.com/premium-vector/large-young-woman-chooses-sport-yoga-jogging-gym-health-weight-loss-infographics-flat-vector-image_22089393.htm
(16) Figure 7 retrieved from https://www.alamy.com/diet-infographic-set-with-effective-tips-of-weight-loss-flat-vector-illustration-image400645121.html?imageid=54649B55-8DC3-4AA1-B57E-9FDE19571BC7&p=1360243&pn=1&searchId=dd9d4f7f708c8d9e36ed684faace773e&searchtype=0
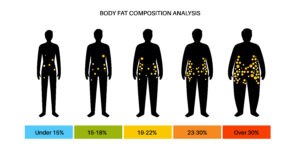
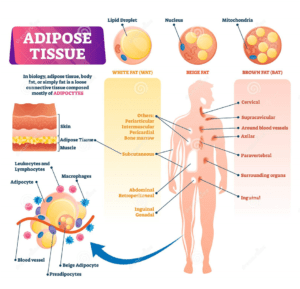

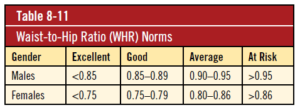 Figure 2 Wait to hip ratio chart (11)
Figure 2 Wait to hip ratio chart (11)