The Relationship Between Obesity and The Cardiovascular System
| The Obesity Dilemma III |
 Obesity is becoming a global epidemic, and there has been a dramatic increase in obesity cases among children and adults in the past 10 years. Obesity is an independent risk factor for cardiovascular disease and is associated with an increased risk of mortality and morbidity. As adipose tissue accumulates in excess amounts, various adaptations occur in cardiac structure and function. On the whole, obesity is associated with various cardiac complications such as coronary heart disease, heart failure, and sudden death because of its impact on the cardiovascular system. (1)
Obesity is becoming a global epidemic, and there has been a dramatic increase in obesity cases among children and adults in the past 10 years. Obesity is an independent risk factor for cardiovascular disease and is associated with an increased risk of mortality and morbidity. As adipose tissue accumulates in excess amounts, various adaptations occur in cardiac structure and function. On the whole, obesity is associated with various cardiac complications such as coronary heart disease, heart failure, and sudden death because of its impact on the cardiovascular system. (1)
Cardiovascular adaptations to obesity
Obesity causes an increase in circulating blood volume to meet the metabolic demands of the enlarged adipose and lean tissue. As a result, blood pressure is elevated, causing high rates of hypertension. The increased filling pressures and volumes increase cardiac workload predisposing obese individuals to an abnormal left ventricular geometry and remodelling. The left ventricle is dilated to accommodate the increased amount of blood. Left ventricular hypertrophy and dysfunction may develop to keep the wall stress normal. The left atrium is also influenced by obesity. Increased blood volume and abnormal left ventricular function may lead to left atrium enlargement, increasing the risk for heart failure and atrial fibrillation. The increased filling pressures in the right side of the heart may lead to mild increases in pulmonary artery systolic pressure. (2)
Cardiovascular impact of increased adipose tissue mass
In obesity, adipose tissue undergoes maladaptive expansion, which compromises its function. Initially, adipocyte hyperplasia occurs, followed by hypertrophy. Angiogenesis is impaired, which causes localized hypoxia and ischemic necrosis. A vicious cycle of inflammatory response occurs.
Adipokines: crossroads between obesity and CVD
Adipokine dysregulation is the prominent hallmark of dysfunctional adipose tissue. Adipokines are secreted by adipose tissue; some are obesity-related low-grade state of inflammation. The peripheral fat deposition has a favorable impact on CVD risk. (2)
Obesity and cardiovascular disease
Duration of obesity and CVD
Research has shown that the alteration of cardiac performance in obese patients with left ventricular enlargement and wall thickening is attributed to the duration of obesity. The authors concluded that the risk of all-cause mortality increased as the number of years lived with obesity increased, independent of current BMI and set of potential cofounders. For every 2 years additionally lived with obesity, the risk of CVD mortality increased by 7%. (3) Hence delaying the onset of obesity can lower the risk of future CVD.
Fat-but-fit paradigm and CVD

Fat-but-fit paradigm refers to those individuals who, despite being obese, have good cardiorespiratory fitness level. Physical activity and physical fitness are closely related to obesity. Research has concluded that being more active was related to a marked reduction in the risk of incident CVD and early mortality. Enough evidence supports that being physically active is related to a lower risk of CVD and longer life expectancy. This evidence applies to both healthy individuals as well as to patients with CVD. (3)
Fat-but-fit and CVD prognosis
Research has concluded that people who are obese but fit have a higher risk of CVD mortality than normal-weight and fit people. On the contrary, this risk is 50% lower than that observed in average weight and unfit people and also dramatically lower than the risk in obese and unfit people. (3)
Figure 1 PATHOPHYSIOLOGY OF OBESITY CARDIOMYOPATHY- this diagram shows the central hemodynamic, cardiac structural abnormalities, and alterations in ventricular function that may occur in severely obese patients and predispose them to heart failure3
This data support 2 public health messages.
- Improving cardiorespiratory fitness without a weight reduction might have long-term benefits.
- An obese person who is fit might have a lower risk of CVD mortality than an average-weight but an unfit person.
Hence physical activity and physical fitness counteract the adverse effects of obesity on the cardiovascular system of man.
Obesity and Hypertension
The mechanisms of obesity-related hypertension and obesity are complex and interdependent. The sympathetic nervous system plays an essential role in affecting renal and adrenal function. (5) The presence of obesity and hypertension in the same individual increases cardiovascular risk. (6)
Sympathetic nervous system and reflex
Obesity shows signs of adrenergic activation, such as increased norepinephrine value. Sympathetic nerve discharge and an increased spillover rate of norepinephrine, particularly at the kidney level, are evident in obese individuals. This is due to impaired arterial baroreceptor control of sympathetic nerve activity. Increased sympathetic outflow to the kidney causes increased renal tubular sodium reabsorption, resulting in increased blood pressure. (5)
Adipokines
Leptin and adiponectin are the most critical products of fatty tissue, which play a role in blood pressure control through the regulation of arterial tone. Leptin reduces appetite and increases energy expenditure by stimulation of nervous system receptors. Levels of these adipokines are reduced in obesity. (5)
Studies have shown that central obesity measured by waist circumference is more closely related to the hypertension phenotype. (6)
Vascular alterations
Obesity and hypertensive state are associated with large artery structure and function alterations. An increase in arterial stiffness and a reduction in arterial compliance and distensibility occurs. (5)
Obesity and vascular dysfunction
Obesity affects the vascular system by altering the function of perivascular adipose tissue (PVAT). The primary role of the cardiovascular system is to transport oxygen and nutrients to organs, tissues, and cells. Dysregulation of the vascular system may result in increased peripheral vascular resistance and blood pressure. Also, vascular dysfunction promotes atherogenesis and increases insulin resistance. (7)
Role of perivascular adipose tissue
Perivascular adipose tissue surrounds large arteries, veins, small vessels, and skeletal muscle microvessels. PVAT plays a role in intravascular thermoregulation. It regulates vascular tone by releasing bioactive molecules, including adipokines, cytokines, and some gaseous molecules. (7)
Obesity has numerous adverse effects on cardiovascular structure and function. Abdominal adiposity is associated with vascular dysfunction. The PVAT mass and adipocyte size are increased, accompanied by other structural modifications in the PVAT. Its anticontractile effect is completely lost in obese patients. 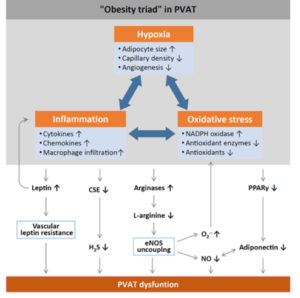
Figure 2 MECHANISMS OF PVAT DYSFUNCTION IN DIET-INDUCED OBESITY7
(7) Based on research results, an ‘obesity triad’ consisting of PVAT hypoxia, inflammation, and oxidative stress can be proposed as the central mechanism in obesity-induced PVAT dysfunction. (7)
Obesity and atherosclerotic vascular disease
Obesity is a multifactorial and chronic disease in which visceral and subcutaneous fat accumulation occurs. Obesity is linked with atherosclerosis through various mechanisms, including abnormalities in lipid metabolism, insulin resistance, inflammation, endothelial dysfunction, and adipokine imbalance. (8)
Adipokine imbalance
Evidence suggests that an imbalance between pro-inflammatory and anti-inflammatory adipokines is responsible for developing endothelial dysfunction and atherosclerosis. (8)
Oxidative stress links obesity to atherosclerosis
Obesity increases systemic oxidative stress. It results from an imbalance between the production of free radicals and anti-oxidant systems. Increased oxidant production increases atherosclerosis susceptibility. (8) The lipid components of low-density lipoproteins (LDL) undergo oxidative modification. LDL deposits in the vascular wall early in the atherosclerotic lesion, where it is oxidized. Oxidized lipids contribute to many stages of atherosclerotic development. (9)
Endothelial dysfunction
Endothelium lines the entire vascular system. Endothelial dysfunction is known to be the earliest clinically detectable form of atherosclerosis. (10) Obesity impairs endothelial function through several mechanisms, including decreased NO production. (8)
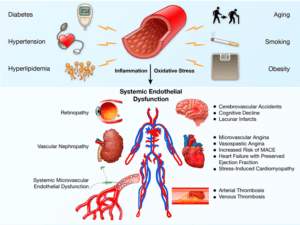
Figure 3 ENDOTHELIAL DYSFUNCTION-A SYSTEMIC DISEASE. Figure represents risk factors and widespread systemic manifestations of vascular endothelial dysfunction
Heart failure and obesity
Obesity is a significant risk factor for the development of heart failure. Research showed that the risk of heart failure increased by 7% for women and 5% for men for each unit increase in BMI. (11)
Mechanism of obese heart failure with a preserved ejection fraction
Obesity is associated with an abundance of renal tubular sodium transporters, overproduction of aldosterone, and activation of the renin-angiotensin axis. It leads to increased sodium reabsorption and plasma volume expansion. Increased blood pressure and blood volume in obesity lead to structural and functional alterations that contribute to heart failure. (12)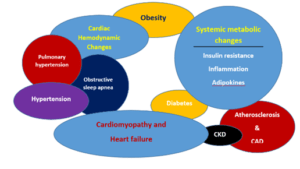
Furthermore, in individuals with obesity, there is a disruption of metabolic homeostasis and excess nutrient supply to the heart. The degree of obesity and adipose tissue location play important roles in the pathophysiology of obese heart failure. Epicardial fat increases pericardial restraint and intracardiac filling pressures in obese individuals with heart failure. (12)
Figure 4 PATHOPHYSIOLOGY OF OBESITY CARDIOMYOPATH
Via the production and release of inflammatory cytokines, epicardial fat can cause microvascular dysfunction and fibrosis of the myocardium. Remodeling and myopathy of the left atrium often lead to the development of atrial fibrillation, which contributes to the pathogenesis of heart failure with preserved ejection fraction in obesity. (12)
Diet quality, energy balance, and obesity
Obesity is challenging to treat after it has developed. Growing evidence suggests that poor diet quality causes energy imbalance. Furthermore, diet quality influences metabolic risk and propensity toward abdominal adiposity. The primary prevention of weight gain is promising for individual patients and populations. Studies suggest no harm of whole-fat milk for obesity or cardiovascular disease. Children who drink low-fat milk habitually gain more weight, and those who drink whole-fat milk gain less weight over time. (4)
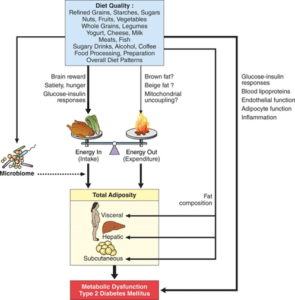
Figure 5 Diet quality, obesity and metabolic risk- a modern paradigm. Diet quality influences risk of adiposity through multiple pathways, including altering energy intake, energy expenditure, microbiome-host interactions, body fat composition and
Exercise to reduce body weight
Increasing daily energy expenditure to tip the energy balance is effective in the treatment of obesity. Energy expenditure can be increased by increasing physical activity. The processes that accelerate the breakdown of the body’s major energy stores (glycogen and triacylglycerols) contribute to energy expenditure leading to weight loss. Exercise speeds up this phenomenon through the stimulated secretion of hormones and changes in substrate concentrations that activate enzymes. (14)
Exercise type should be taken into account in the treatment of obesity. Endurance exercise is the most popular exercise for body weight loss. Achieving significant weight loss in obesity is only the half job. Weight regain is common, and even a mild degree of weight increase seems to reverse the benefits of weight loss. Studies have shown that interventions combining diet and exercise result in smaller weight regain. (14)
References
- Poirier, P., Giles, T. D., Bray, G. A., Hong, Y., Stern, J. S., Pi-Sunyer, F. X., & Eckel, R. H. (2006). Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation, 113(6), 898-918.
- Koliaki, C., Liatis, S., & Kokkinos, A. (2019). Obesity and cardiovascular disease: revisiting an old relationship. Metabolism: clinical and experimental, 92, 98–107. https://doi.org/10.1016/j.metabol.2018.10.011
- Ortega, F. B., Lavie, C. J., & Blair, S. N. (2016). Obesity and cardiovascular disease. Circulation research, 118(11), 1752-1770.
- Mozaffarian D. (2016). Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation, 133(2), 187–225. https://doi.org/10.1161/CIRCULATIONAHA.115.018585
- Seravalle, G., & Grassi, G. (2017). Obesity and hypertension. Pharmacological research, 122, 1–7. https://doi.org/10.1016/j.phrs.2017.05.013
- Ruilope, L. M., Nunes Filho, A., Nadruz, W., Jr, Rodríguez Rosales, F. F., & Verdejo-Paris, J. (2018). Obesity and hypertension in Latin America: Current perspectives. Hipertension y riesgo vascular, 35(2), 70–76. https://dRuilope, L. M., Nunes Filho, A., Nadruz, W., Jr, Rodríguez Rosales, F. F., & Verdejo-Paris, J. (2018). Obesity and hypertension in Latin America: Current perspectives. Hipertension y riesgo vascular, 35(2), 70–76. https://doi.org/10.1016/j.hipert.2017.12.004oi.org/10.1016/j.hipert.2017.12.004
- Xia, N., & Li, H. (2017). The role of perivascular adipose tissue in obesity‐induced vascular dysfunction. British journal of pharmacology, 174(20), 3425-3442.
- Lovren, F., Teoh, H., & Verma, S. (2015). Obesity and atherosclerosis: mechanistic insights. Canadian Journal of Cardiology, 31(2), 177-183.
- Morrow, J. D. (2003). Is oxidant stress a connection between obesity and atherosclerosis?. Arteriosclerosis, thrombosis, and vascular biology, 23(3), 368-370.
- Corban, M. T., Lerman, L. O., & Lerman, A. (2019). Endothelial dysfunction: cardiovascular disease pathophysiology hidden in plain sight. Arteriosclerosis, thrombosis, and vascular biology, 39(7), 1272-1274.
- Horwich, T. B., Fonarow, G. C., & Clark, A. L. (2018). Obesity and the Obesity Paradox in Heart Failure. Progress in cardiovascular diseases, 61(2), 151–156. https://doi.org/10.1016/j.pcad.2018.05.005
- Koutroumpakis, E., Kaur, R., Taegtmeyer, H., & Deswal, A. (2021). Obesity and Heart Failure with Preserved Ejection Fraction. Heart failure clinics, 17(3), 345–356. https://doi.org/10.1016/j.hfc.2021.02.003
- https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25434909
- Petridou, A., Siopi, A., & Mougios, V. (2019). Exercise in the management of obesity. Metabolism: clinical and experimental, 92, 163–169. https://doi.org/10.1016/j.metabol.2018.10.009