Strategies and Lifestyle habits to address the obesity problem
|
The Obesity Dilemma IV |

The development of guidelines for obesity is complex. It involves both treatment interventions and interventions related to screening and prevention. Obesity is the most chronic metabolic disease worldwide. The WHO has already declared it a global epidemic. In the European region, obesity presents an unprecedented and underestimated public health challenge. Despite steady progress in managing obesity, the prevalence of obesity continues to rise, stressing the necessity for prevention strategies at the individual and community level. (2)
Comprehensive Obesity Management
The management and treatment of obesity include weight loss, risk reduction, and health improvement. It can be achieved by modest weight reduction (i-e 5-10% of initial body weight), improved nutritional content of the diet, and an increase in physical activity and fitness. (2)
Where someone with the risk of obesity should turn to for solutions
Setting the right eating habits is a basic pillar of the non-pharmacological treatment of obesity. (15) If you are susceptible to the risk of obesity, you can go to a dietitian, nutritionist, behavioral counselor, or an obesity specialist. They will help you understand and change your eating and activity habits. They will tell you your daily calorie requirement so that you can lose weight steadily. This will help you to make positive and healthy lifestyle changes.
The benefits of weight loss
Evidence suggests that the risks of mortality and morbidity associated with obesity can be reduced effectively with weight loss. (1) Weight loss results in a short-term decrease in blood pressure. (3) research has shown that a 5-10% weight loss of pretreatment body weight has been associated with significant improvements in medical disorders such as type 2 diabetes, hypertension, and cardiovascular disease. It also results in an increase in life span. (1)
Prevention of obesity
Adequate management of obesity is essential and requires the principles of integrated care for disease management. The standard principle of management is early detection, diagnosis, and treatment of obesity. The preferred treatment is a combined lifestyle intervention and, when appropriate, additional medical therapies. Individuals respond to local environmental factors like socio-cultural, economic, and physical environments. (5)
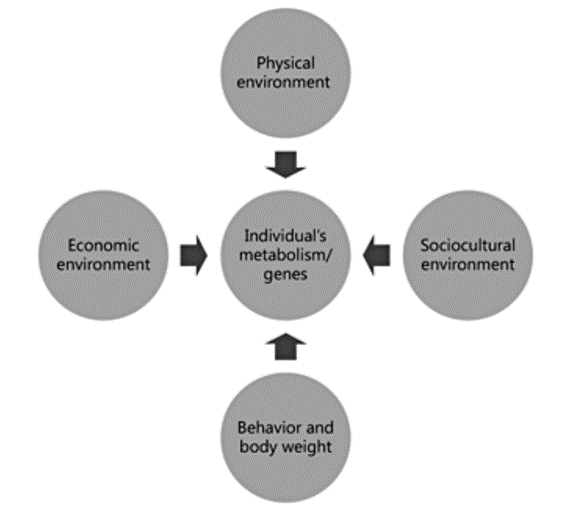
Figure1: Representation of environmental influences interacting with individuals and the effects on behavior and body weight
Biological and socioenvironmental (economics, culture, social networks, and physical environment) influences on behaviors such as eating and physical activity play a role in obesity prevention. (5)
Consulting with the GP to address the problem of obesity
If you notice a change in your body weight, you should consult with your GP. Your GP will guide you to overcome the problem of obesity.
Latest guidelines for obesity management
In 2013, the National Health and Medical Research Council (NHMRC) released updated clinical practice guidelines for the management of obesity in primary care. General Practitioners are encouraged to use the ‘5As’ to manage patients’ weight. These are Ask, Assess, Advise, Assist and Arrange. The new guidelines also follow a patient-centered approach, with the intention that the patient will be involved in the planning and implementation of their weight management. (9)
Socioeconomic Challenge of Obesity
Obesity prevalence is increasing at an alarming rate worldwide. Based on the existing prevalence and trend data, it is reasonable to describe obesity as a public health crisis. It affects people’s health and quality of life and adds to the healthcare budget. (5)
The economic cost of obesity
Given the high prevalence and the significant health risks associated with obesity, the economic costs of obesity have been estimated to be 3-8% of the total healthcare expenditure. Most of the cost arises from treating hypertension, coronary heart disease, and type 2 diabetes. The indirect cost is in terms of lost output in the economy due to sickness absence or premature death. (1)
Shifting the burden of obesity toward the poor
The prevalence of obesity is higher in low and middle-income countries. (5) Statistical analyses were carried out, and the relative annual change in weighted prevalence of obesity is higher for rural than urban women. The analyses show that increased per-capita GDP is associated with an increased prevalence of overweight and obesity in rural areas. (4)
Special concerns for low and middle-income countries
The patterns of change in dietary intake and energy expenditure are essential in the development of obesity. Fetal nutritional insufficiency triggers anatomical, hormonal, and physiological changes that enhance survival in a resource-poor environment. These adaptations may contribute to disease development with plentiful resources in the postnatal environment. Maternal exposure to famine conditions causes moderate to severe nutrition restriction during pregnancy. Studies show that there is a role of maternal micronutrient intake in epigenetic changes that affect child adiposity. There is also evidence that maternal overweight and obesity in pregnancy influence disease risk among offspring. (4)
Obesity and Genetics
The general public believes that body weight is within personal control. This concept worsens attitudes towards obese persons. New research findings illustrate that obesity has a significant genetic component. (6) This could increase awareness of an important uncontrollable element of obesity. This finding can reduce the obesity stigma among healthy-weight people.
Role of genes in obesity
Genetics plays a substantial role in the predisposition to obesity. It may contribute to up to 70% risk for the disease. Over a hundred genes and gene variants related to excess weight have been discovered, but genetic obesity does not always cause obesity development. There are complex interactions between genetic, behavioral, and environmental influences and resulting epigenetic changes. Monogenic obesity though rare, typically appears in early childhood. Polygenic obesity is the most common and demonstrates the interplay between genes and the obesogenic environment. (7)
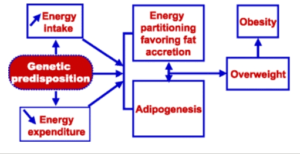
Figure 2: Determinants of positive energy balance and fat deposition with an indication of the sites of action of a genetic disposition
Evidence from genetic epidemiology
Research has shown that the prevalence of obesity (BMI 30) is twice as high in families of obese individuals than in the population at large. Moreover, the risk of extreme obesity (BMI 45) is about seven to eight times higher in families of extremely obese individuals. (8)
Genome-wide-scans for obesity-related phenotypes
Genome-wide scans can be used to detect chromosomal regions showing linkage with obesity. Genetic screening for obesity concentrates on identifying mutations in specific genes in persons who are severely obese, with the greatest success rates in cases with an early onset. (8)
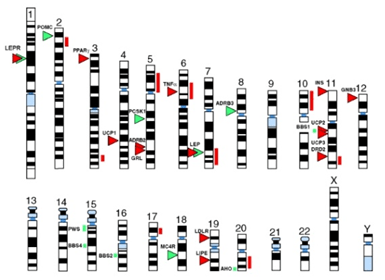
Figure 3 Chromosomal location of obesity
Contribution of Ethnicity toward Perception of Obesity
Racial or ethnic composition is an important correlate of obesity risk. Environmental and social norms that operate within communities and ethnic groups play an essential role in the development of obesity. (10)
The reasons for ethnic variation in obesity are complex. They may include differences in cultural beliefs and practices, perceptions of media, sleep, physical activity, level of acculturation, and ethnicity-based differences in body image. (11)
Factors affecting ethnicity toward obesity
Cultural beliefs and practices may contribute to racial disparities in obesity. Different cultures have different parental perceptions about their children’s health status and behaviors. In some cultures, mothers may view thinness as a reflection of malnutrition and poor health. Culturally defined perceptions of body image influence parenting strategies regarding eating and physical activity habits. (11)
Personal Responsibility towards Obesity
The regulation of hunger and satiety is poor in today’s obesogenic environment. A variety of factors lead to the risk of arriving at a pathological state of obesity. Sedentariness, food culture impacting seasonal weight gain, poor sleep, stress, energy-dense foods, genetic factors, and certain medications increase the risk of weight gain and obesity. (12)
Conscious experience and appetite regulation
Our brain is the most complex organ responsible for generating conscious experience. Individuals are free to choose how much they want to weigh. Appetite sensations are generated by the subcortical areas such as the hypothalamus and area postrema. (12)
For some individuals, the drive to eat may be greater than the ability to manage this drive. This can and should be managed solely by individuals’ willpower. (12)
Measures for prevention of obesity

Optimizing nutrition and growth in infancy and establishing healthy lifestyles can help reduce the risk of obesity. Interventions targeting infant feeding, parenting styles, diet, and physical activity in preschool children can reduce obesity risk. Interactive programs in group settings are likely to engage families. These programs should meet the needs of families and children. Programs that are fun, interactive, and able to engage parents and children are likely to be successful. Interventions should begin in infancy and continue through preschool years for maximum chances of success. (13)
Why the strategies adopted by society have failed
Many challenges are encountered while implementing successful interventions on a large scale. These include a lack of resources, participation of parents in community-based programs, socioeconomic factors, and financial, time-related, and social costs. Additional cost related to buying healthier foods and adopting a healthier lifestyle is a big challenge. Understanding these problems would help implement interventions and increase their success chances. (13)
Cost-Effectiveness of considering a prevention approach
We can deal with the problem of obesity through different approaches. The prevention approach is better than reacting to the problem. It is cost-effective and a healthy approach. Obesity-related chronic conditions are preventable and should be amenable to prevention strategies and programs. (14) If the susceptible individuals follow the interventions and successfully prevent obesity, they will not have to go through expensive treatment options. It would not only be healthy for them but also would not burden the healthcare system.
Effect of Obesity on the Current Healthcare
Obese individuals often have preventable chronic conditions. The management and treatment of chronic conditions related to obesity require higher utilization of medical services. The higher utilization of services leads to largely preventable costs. Emphasis on health management for obese individuals targeting lifestyle behaviors and weight management can help reduce costs for the individual and Medicare. (14)
References
- Labib, M. J. J. o. C. P. (2003). The investigation and management of obesity. 56(1), 17-25
- Tsigos, C., Hainer, V., Basdevant, A., Finer, N., Fried, M., Mathus-Vliegen, E., . . . Schutz, Y. J. O. f. (2008). Management of obesity in adults: European clinical practice guidelines. 1(2), 106-116.
- Aucott, L., Poobalan, A., Smith, W. C. S., Avenell, A., Jung, R., & Broom, J. (2005). Effects of weight loss in overweight/obese individuals and long-term hypertension outcomes: a systematic review. Hypertension, 45(6), 1035-1041.
- Popkin, B. M., Adair, L. S., & Ng, S. W. (2012). Global nutrition transition and the pandemic of obesity in developing countries. Nutrition reviews, 70(1), 3–21. https://doi.org/10.1111/j.1753-4887.2011.00456.x
- Seidell, J. C., & Halberstadt, J. (2015). The global burden of obesity and the challenges of prevention. Annals of nutrition & metabolism, 66 Suppl 2, 7–12. https://doi.org/10.1159/000375143
- Lippa, N. C., & Sanderson, S. C. (2013). Impact of informing overweight individuals about the role of genetics in obesity: an online experimental study. Human Heredity, 75(2-4), 186–203. https://doi.org/10.1159/000353712
- Golden, A., & Kessler, C. (2020). Obesity and genetics. Journal of the American Association of Nurse Practitioners, 32(7), 493-496.
- Loos, R. J., & Bouchard, C. (2003). Obesity–is it a genetic disorder?. Journal of internal medicine, 254(5), 401-425.
- Jansen, S., Desbrow, B., & Ball, L. (2015). Obesity management by general practitioners: the unavoidable necessity. Australian journal of primary health, 21(4), 366–368. https://doi.org/10.1071/PY15018
- Kirby, J. B., Liang, L., Chen, H. J., & Wang, Y. (2012). Race, place, and obesity: the complex relationships among community racial/ethnic composition, individual race/ethnicity, and obesity in the United States. American journal of public health, 102(8), 1572-1578.
- Peña, M. M., Dixon, B., & Taveras, E. M. (2012). Are you talking to ME? The importance of ethnicity and culture in childhood obesity prevention and management. Childhood obesity (Print), 8(1), 23–27. https://doi.org/10.1089/chi.2011.0109
- Grannell, A., Fallon, F., Al-Najim, W., & le Roux, C. (2021). Obesity and responsibility: Is it time to rethink agency?. Obesity reviews: an official journal of the International Association for the Study of Obesity, 22(8), e13270. https://doi.org/10.1111/obr.13270
- Lanigan J. (2018). Prevention of overweight and obesity in early life. The Proceedings of the Nutrition Society, 77(3), 247–256. https://doi.org/10.1017/S0029665118000411
- Musich, S., MacLeod, S., Bhattarai, G. R., Wang, S. S., Hawkins, K., Bottone, F. G., Jr, & Yeh, C. S. (2016). The Impact of Obesity on Health Care Utilization and Expenditures in a Medicare Supplement Population. Gerontology & geriatric medicine, 2, 2333721415622004. https://doi.org/10.1177/2333721415622004
- Sadílková, A., Čmerdová, K., & Hásková, A. (2020). Role of dietitian in obese patients care. Úloha nutričního terapeuta v péči o obézní. Casopis lekaru ceskych, 159(3-4), 131–135.